References
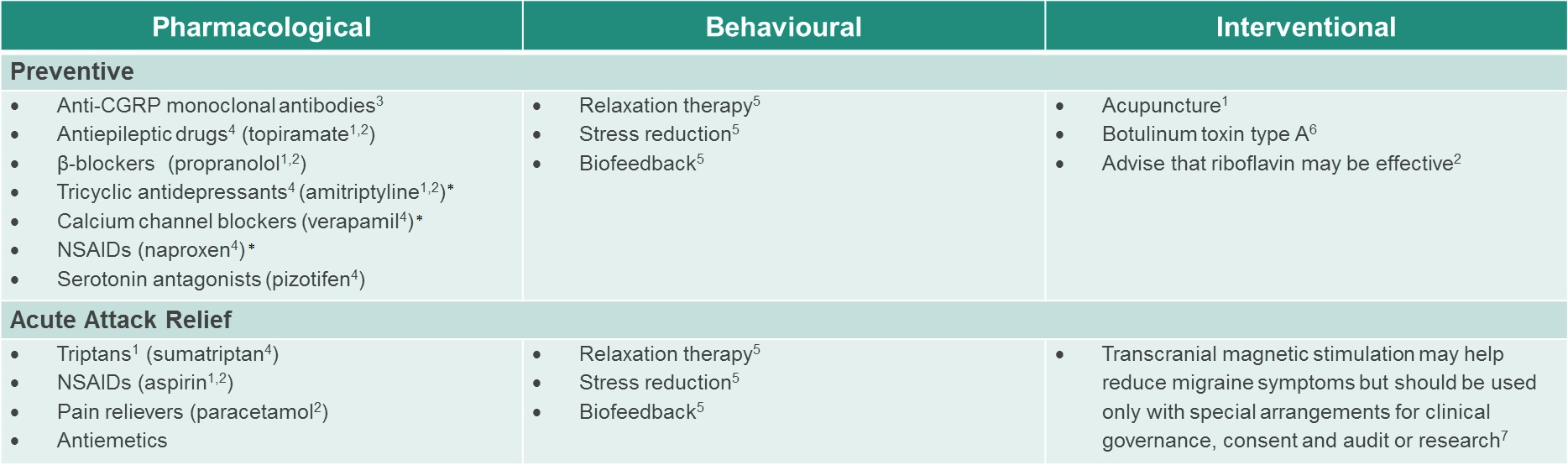
1. Silberstein SD. Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2000; 55(6): 754–762
2. National Institute for Health and Care Excellence. Headaches in over 12s: diagnosis and management. Clinical guideline 150. September 2012 (updated 2015)
3. Charles A, Pozo-Rosich P. Targeting calcitonin gene-related peptide: a new era in migraine therapy. Lancet 2019; 9; 394(10210):1765-1774;
4. Antonaci F et al. A review of current European treatment guidelines for migraine. J Headache Pain 2010; 11: 13–19
5. British Association for the Study of Headache. Guidelines for all healthcare professionals in the diagnosis and management of Migraine. 3rd edition. September 2010
6. National Institute for Health and Care Excellence. Botulinum toxin type A for the prevention of headaches in adults with chronic migraine. Technology appraisal guidance 260. June 2012
7. National Institute for Health and Care Excellence. Transcranial magnetic stimulation for treating and preventing migraine. Interventional procedures guidance IPG477. January 2014
8. Lipton RB, Silberstein SD. Episodic and chronic migraine headache: breaking down barriers to optimal treatment and prevention. Headache 2015; 55 (Suppl 2): 103–122
9. Bigal ME, Lipton RB. Clinical course in migraine: conceptualizing migraine transformation. Neurology 2008; 71(11): 838–855
10. Bigal ME, Lipton RB. Overuse of acute migraine medications and migraine chronification. Curr Pain Headache Rep 2009; 13: 301–307
11. American Migraine foundation. Headache Hygiene - What is it? 2016 Available at: https://americanmigrainefoundation.org/understanding-migraine/headache-hygiene-what-is-it/ (last accessed September 2018)
12. Al-kotb H and Ibrahim MH. American Journal of Nursing Science 2016;5:280–287
13. Ray, J. et al The state of migraine: An update on current and emerging treatments, Australian Journal for General Practitioners 2021; 50: 915-921]